Neurosurgical Intervention in Ischaemic Stroke: A Case Report
Dr S S Ahmed, Dr Chaity Nath, Dr Al Imran
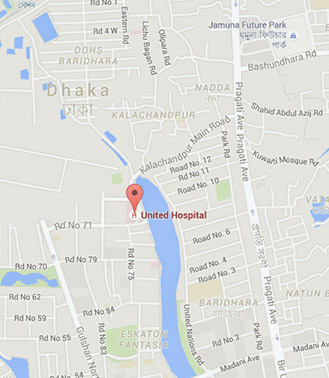
A normotensive and non-diabetic 60 year old gentleman was admitted in United Hospital ICU through Accident & Emergency department with history of vertigo and vomiting followed by loss of consciousness for 4 days prior admission. There was no history of convulsion. After admission, his pulse rate was 71 beat/min, blood pressure was 150/90 mm of Hg, temp above 98ºF, SpO2 97% in room air with no abnormality detected in heart/lung. On neurological examination, GCS was 6T/15 (E3M3VT),Pupil was 2.5 mm equal & reacting to light with no neck rigidity. All jerks were brisk & planter responses were extensor, bilaterally. However, patient was being treated conservatively, his GCS was deteriorating and a repeat CT scan and MRI of brain showed extensive acute infarction involving both cerebellums,basal ganglia, brainstem with midline shifting with obstructive hydrocephalus. He was transferred from neuromedicine to neurosurgery department; he underwent urgent posterior fossa suboccipitalcraniotomy and duroplasty. Post-operatively his clinical condition gradually improved and he was transferred to ward after 10 days of ICU stay. He required insertion of PEG tube for feeding and was discharged after which he was treated in a local hospital. At 2 months of follow up, at United Hospital, his CNS function was found to be significantly improved and he was taking food normally. Later PEG tube was removed and on further follow up after one month, he was found walking without support and he was able to communicate normally. In patients with ischaemic stroke, having acute infarction involving critical brain area, fatality can be avoided if diagnosed earlier with prompt surgical intervention thereafter.