Placenta Accreta-A Growing Concern in Recent Obstetric Practice
Placenta Accreta--A Growing Concern in Recent Obstetric Practice
Dr Nusrat Zaman, Dr Afsari Ahmad
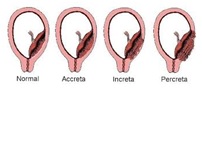 Placenta accreta is a severe complication and is currently the most common indication for peripartum hysterectomy. Placenta accreta occurs when the chorionic villi invade the myometrium abnormally. It is divided into three grades based on histopathology; placenta accreta where the chorionic villi are in contact with the myometrium, placenta increta where the chorionic villi invade the myometrium, and placenta percreta where the chorionic villi penetrate the uterine serosa. It is becoming an increasingly common complication mainly due to the increasing rate of caesarean delivery, as placenta tends to implant in the lower uterine segment specially over the previous caesarean scar; it gets more severe particularly when accompanied with a coexisting placenta praevia.
Placenta accreta is a severe complication and is currently the most common indication for peripartum hysterectomy. Placenta accreta occurs when the chorionic villi invade the myometrium abnormally. It is divided into three grades based on histopathology; placenta accreta where the chorionic villi are in contact with the myometrium, placenta increta where the chorionic villi invade the myometrium, and placenta percreta where the chorionic villi penetrate the uterine serosa. It is becoming an increasingly common complication mainly due to the increasing rate of caesarean delivery, as placenta tends to implant in the lower uterine segment specially over the previous caesarean scar; it gets more severe particularly when accompanied with a coexisting placenta praevia.
 Antenatal diagnosis can be achieved by ultrasound in the majority of cases. MRI also assists to know the extent of placental invasion to urinary bladder or adjacent lateral pelvic wall. Women with placenta accreta are usually delivered by elective caesarean section. In order to avoid an emergency caesarean section and to minimize complication of prematurity it is acceptable to schedule caesarean at 34 to 35 weeks. In third world countries like ours, it is acceptable to deliver at 36 completed weeks if patient is stable or earlier if alarming bleeding appears. Since, placenta accreta is most likely to affect the urinary bladder and general anaesthesia may be the most appropriate choice in majority of the cases, hence multidisciplinary team approach with senior obstetrician, senior anesthesiologist and urologist and delivery at a center with adequate resources, including those for massive transfusion are essential to reduce neonatal and maternal morbidity and mortality. ICU facility may also be required for post-operative management of mother and NICU facility for preterm neonate. Caesarean hysterectomy is probably the preferable and acceptable treatment. In carefully selected cases, when fertility is desired, conservative management may be considered with caution. Post-operative Methotrexate is used in some cases of placenta accreta where uterus is preserved.
Antenatal diagnosis can be achieved by ultrasound in the majority of cases. MRI also assists to know the extent of placental invasion to urinary bladder or adjacent lateral pelvic wall. Women with placenta accreta are usually delivered by elective caesarean section. In order to avoid an emergency caesarean section and to minimize complication of prematurity it is acceptable to schedule caesarean at 34 to 35 weeks. In third world countries like ours, it is acceptable to deliver at 36 completed weeks if patient is stable or earlier if alarming bleeding appears. Since, placenta accreta is most likely to affect the urinary bladder and general anaesthesia may be the most appropriate choice in majority of the cases, hence multidisciplinary team approach with senior obstetrician, senior anesthesiologist and urologist and delivery at a center with adequate resources, including those for massive transfusion are essential to reduce neonatal and maternal morbidity and mortality. ICU facility may also be required for post-operative management of mother and NICU facility for preterm neonate. Caesarean hysterectomy is probably the preferable and acceptable treatment. In carefully selected cases, when fertility is desired, conservative management may be considered with caution. Post-operative Methotrexate is used in some cases of placenta accreta where uterus is preserved.
A 35 year old lady in her third pregnancy (gravida 3) was admitted in United Hospital at 36+ weeks of pregnancy with central placenta praevia with placenta accreta with history of two previous caesarian sections. Patient gave consent for hysterectomy if required. The baby was delivered by caesarian section with upper segment incision and placenta was kept in situ. Placenta accreta was found completely encroaching the anterior uterine wall, bladder and right broad ligament. Profuse haemorrhage extending up to right broad ligament was observed which was controlled by clamping all vessels. During this procedure clamp was given in right infundibulopelvic ligament and total abdominal hysterectomy was done. Some placental tissue encroaching up to base of bladder were seen. Urinary bladder showed no rent. Both ureters were checked. Continuous catheter and a drain tube were kept. Postoperative recovery was uneventful. Patient got total 5 units of whole blood. Catheter was kept for 7 days and patient was ready to be discharged from hospital.
On 7th post-operative day she developed paralytic ileus and her abdomen was distended. Ultrasound showed mild collection in pelvis. Patient was evaluated by Urologist and General Surgeon. Decision was taken to remove pelvic collection. Ultrasonography guided peritoneal fluid aspiration was done and a pigtail drain was kept in situ as fresh uriniferous collection was detected in pelvis. Cystoscopic evaluation was done, later which revealed no injury. D-J stenting was done. Bladder wall showed sloughing out of placental necrotic tissue in small areas of bladder mucosa within bladder lumen. There was retained placental tissue in the dome of urinary bladder.
Decision of relaparotomy was immediately taken to remove all placental dead tissue. Stump in vault showed no abnormalities. All dead necrotic tissue were removed from the dome of the bladder. Then dome of the bladder was repaired in 2 layers. A drain tube was kept in pelvis. Continuous trichannel catheter was given for irrigation and drainage.
Meanwhile all possible supportive treatments such as albumin infusion, blood transfusion and high protein diet were being given to patient; with review by Urologist and Medicine Consultant. After 10 days of relaparotomy, pelvic drain tube was removed. Patient was advised to keep catheter for another 2 weeks; patient was discharged on 16th day post relaparotomy.
Prenatal diagnosis of Placenta accreta seems to be a key factor in optimizing the counseling, treatment and outcome of women with this condition.


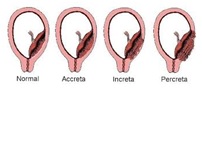 Placenta accreta is a severe complication and is currently the most common indication for peripartum hysterectomy. Placenta accreta occurs when the chorionic villi invade the myometrium abnormally. It is divided into three grades based on histopathology; placenta accreta where the chorionic villi are in contact with the myometrium, placenta increta where the chorionic villi invade the myometrium, and placenta percreta where the chorionic villi penetrate the uterine serosa. It is becoming an increasingly common complication mainly due to the increasing rate of caesarean delivery, as placenta tends to implant in the lower uterine segment specially over the previous caesarean scar; it gets more severe particularly when accompanied with a coexisting placenta praevia.
Placenta accreta is a severe complication and is currently the most common indication for peripartum hysterectomy. Placenta accreta occurs when the chorionic villi invade the myometrium abnormally. It is divided into three grades based on histopathology; placenta accreta where the chorionic villi are in contact with the myometrium, placenta increta where the chorionic villi invade the myometrium, and placenta percreta where the chorionic villi penetrate the uterine serosa. It is becoming an increasingly common complication mainly due to the increasing rate of caesarean delivery, as placenta tends to implant in the lower uterine segment specially over the previous caesarean scar; it gets more severe particularly when accompanied with a coexisting placenta praevia. Antenatal diagnosis can be achieved by ultrasound in the majority of cases. MRI also assists to know the extent of placental invasion to urinary bladder or adjacent lateral pelvic wall. Women with placenta accreta are usually delivered by elective caesarean section. In order to avoid an emergency caesarean section and to minimize complication of prematurity it is acceptable to schedule caesarean at 34 to 35 weeks. In third world countries like ours, it is acceptable to deliver at 36 completed weeks if patient is stable or earlier if alarming bleeding appears. Since, placenta accreta is most likely to affect the urinary bladder and general anaesthesia may be the most appropriate choice in majority of the cases, hence multidisciplinary team approach with senior obstetrician, senior anesthesiologist and urologist and delivery at a center with adequate resources, including those for massive transfusion are essential to reduce neonatal and maternal morbidity and mortality. ICU facility may also be required for post-operative management of mother and NICU facility for preterm neonate. Caesarean hysterectomy is probably the preferable and acceptable treatment. In carefully selected cases, when fertility is desired, conservative management may be considered with caution. Post-operative Methotrexate is used in some cases of placenta accreta where uterus is preserved.
Antenatal diagnosis can be achieved by ultrasound in the majority of cases. MRI also assists to know the extent of placental invasion to urinary bladder or adjacent lateral pelvic wall. Women with placenta accreta are usually delivered by elective caesarean section. In order to avoid an emergency caesarean section and to minimize complication of prematurity it is acceptable to schedule caesarean at 34 to 35 weeks. In third world countries like ours, it is acceptable to deliver at 36 completed weeks if patient is stable or earlier if alarming bleeding appears. Since, placenta accreta is most likely to affect the urinary bladder and general anaesthesia may be the most appropriate choice in majority of the cases, hence multidisciplinary team approach with senior obstetrician, senior anesthesiologist and urologist and delivery at a center with adequate resources, including those for massive transfusion are essential to reduce neonatal and maternal morbidity and mortality. ICU facility may also be required for post-operative management of mother and NICU facility for preterm neonate. Caesarean hysterectomy is probably the preferable and acceptable treatment. In carefully selected cases, when fertility is desired, conservative management may be considered with caution. Post-operative Methotrexate is used in some cases of placenta accreta where uterus is preserved.