A Case of Cervical Lymph Node Tuberculosis in a health care worker: An Emergency Department diagnostic and administrative challenge
Dr Abdullah Al Farook
 A 35 year old male health care worker came to the Emergency Department with complaints of painful and tender left supraclavicular swelling. He did not have fever, chills, night sweats and weight loss. He had no stated history of pulmonary tuberculosis or gastric cancer, but he was administered BCG vaccine as a child. He also had no history of prior exposure to a TB infected person. On physical exam he had a 3X4cm² tender, red, fluctuant swelling in his left supraclavicular area with no tonsillar or other neck lymph node enlargement. The rest of his physical examination was unremarkable.
A 35 year old male health care worker came to the Emergency Department with complaints of painful and tender left supraclavicular swelling. He did not have fever, chills, night sweats and weight loss. He had no stated history of pulmonary tuberculosis or gastric cancer, but he was administered BCG vaccine as a child. He also had no history of prior exposure to a TB infected person. On physical exam he had a 3X4cm² tender, red, fluctuant swelling in his left supraclavicular area with no tonsillar or other neck lymph node enlargement. The rest of his physical examination was unremarkable.
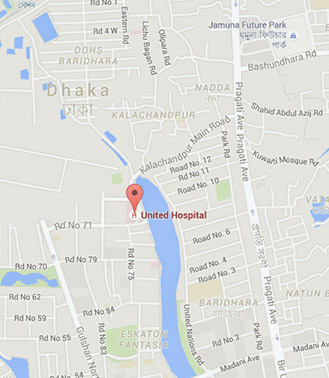
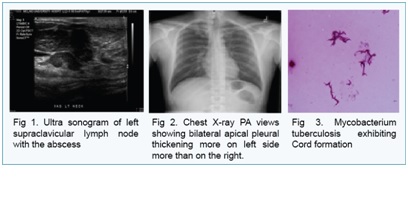
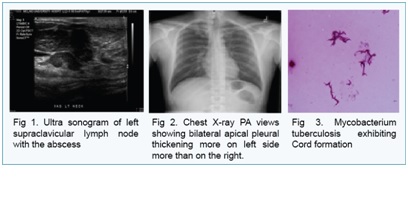
His treatment was started on oral Cotrimoxazol and Clindamycin therapy assuming bacterial infection and a PPD (Purified Protein Derivative) was placed. Two days later PPD was read as positive (>20mm) and Chest X-Ray was negative. USG guided FNA and biopsy of the lymph node showed acute inflammatory exudates, suggestive of acute lymphadenitis. Incision and drainage of the abscess was done at the Emergency Department with follow up appointments. Three weeks later his culture report became positive for Mycobacterium Tuberculosis. He was isolated from the hospital work place and treatment started on DOTS (Directly Observed Treatment Short course) and followed at a local TB Clinic. For him to be infection free, his sputum had to be negative for AFB smears three times both at TB Clinic and at his hospital before he was allowed to return to his work after a period of one month.
Tuberculous cervical lymphadenitis is the commonest presentation of tuberculous infection. It is a diagnostic challenge because it can mimic any other disease of cervical lymph nodes. So, constitutional symptoms and Chest X-Ray are not always positive to help us to diagnose a lymph node TB. A high index of clinical suspicion is required to guide through the differentials.
Original article was presented as a poster at Louisiana State University, University Hospital, New Orleans, USA. Oral presentation was done at South East Society of Academic Emergency Medicine conference, University of Alabama.


 A 35 year old male health care worker came to the Emergency Department with complaints of painful and tender left supraclavicular swelling. He did not have fever, chills, night sweats and weight loss. He had no stated history of pulmonary tuberculosis or gastric cancer, but he was administered BCG vaccine as a child. He also had no history of prior exposure to a TB infected person. On physical exam he had a 3X4cm² tender, red, fluctuant swelling in his left supraclavicular area with no tonsillar or other neck lymph node enlargement. The rest of his physical examination was unremarkable.
A 35 year old male health care worker came to the Emergency Department with complaints of painful and tender left supraclavicular swelling. He did not have fever, chills, night sweats and weight loss. He had no stated history of pulmonary tuberculosis or gastric cancer, but he was administered BCG vaccine as a child. He also had no history of prior exposure to a TB infected person. On physical exam he had a 3X4cm² tender, red, fluctuant swelling in his left supraclavicular area with no tonsillar or other neck lymph node enlargement. The rest of his physical examination was unremarkable.